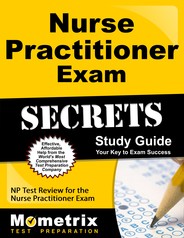
- Family Nurse Practitioner Certification
- Pediatric Nurse Practitioner Certification
- Family Psychiatric & Mental Health Nurse Practitioner Certification
Nurse Practitioner Certification Exam Review Video
Nurse Practitioner Certification Exam Tips & Tricks: Needle and Syringe
Prepare with our Nurse Practitioner Certification Exam Study Guide and Practice Questions. Print or eBook. Guaranteed to raise your score. Get started today!
Nurse Practitioner Certification Exam Flashcards. Proven flashcards raise test scores on the Nurse Practitioner Certification Exam. Guaranteed.
Free Nurse Practitioner Certification Practice Test Questions
1. A nurse practitioner has been assigned a patient who has recently been diagnosed with Guillain- Barre’ Syndrome. Which of the following statements is the most applicable when discussing the impairments with Guillain-Barre’ Syndrome with the patient?
- Guillain-Barre’ Syndrome gets better after 5 years in almost all cases.
- Guillain-Barre’ Syndrome causes limited sensation in the abdominal region.
- Guillain-Barre’ Syndrome causes muscle weakness in the legs.
- Guillain-Barre’ Syndrome does not affect breathing in severe cases.
2. 46 year-old has returned from a heart catheterization and wants to get up to start walking 3 hours after the procedure. The nurse practitioner should:
- Tell the patient to remain with the leg straight for at least another hour and check the chart for activity orders.
- Allow the patient to begin limited ambulation with assistance.
- Recommend a physical therapy consultation for ambulation.
- Tell the patient to remain with leg straight for another 6 hours and check the chart for activity orders.
3. A nurse practitioner is assessing a 18 year-old female who has recently suffered a TBI. The nurse practitioner notes a slower pulse and impaired respiration. The nurse practitioner should report these findings immediately to the physician, due to the possibility the patient is experiencing which of the following conditions?
- Increased intracranial pressure
- Increased function of cranial nerve X
- Sympathetic response to activity
- Meningitis
4. A patient has been diagnosed with diabetes mellitus. Which of the following is not a clinical sign of diabetes mellitus?
- Polyphagia
- Polyuria
- Metabolic acidosis
- Lower extremity edema
5. A patient has fallen off a bicycle and fractured the head of the proximal fibula. A cast was placed on the patient’s lower extremity. Which of the following is the most probable result of the fall?
- Peroneal nerve injury
- Tibial nerve injury
- Sciatic nerve injury
- Femoral nerve injury
Nurse Practitioner Certification Answer Key
1. Answer: C
Muscle weakness in the lower extremities is found in acute cases of Guillain-Barre’ Syndrome.
2. Answer: A
The patient should keep the leg straight for at least 4 hours.
3. Answer: A
The patient is at high risk of developing increased intracranial pressure (ICP).
4. Answer: D
A-C are associated with diabetes mellitus.
5. Answer: A
The head of the proximal fibula is in close proximity to the peroneal nerve.



 Get Your Study Guide
Get Your Study Guide Get Your Flashcards
Get Your Flashcards